Obesity and gestational diabetes mellitus (GDM) are common comorbidities affecting women during pregnancy, including women with asthma. Both conditions are independently associated with adverse pregnancy outcomes, with a combined impact greater than either morbidity alone (Catalano et al. 2012). The presence of either obesity or GDM may present additional considerations in the management of pregnant women with asthma. These include:
- Additional asthma monitoring given the increased risk of exacerbation in pregnancy
- Additional monitoring for adverse pregnancy outcomes associated with both obesity/GDM and asthma
- Monitoring of gestational weight gain to keep within recommended limits
Overweight and obesity
A high proportion of pregnant women with asthma are carrying excess weight, with as many as 7 in 10 women being overweight and obese (Jensen et al. 2020) – this is approximately double the general (Australian) pregnant population rate of 34% (Callaway et al. 2006). In addition to the immediate risks associated with overweight and obesity in pregnancy, including gestational diabetes mellitus (GDM), hypertensive disorders, and preterm birth (Das et al. 2021), particular considerations are required in the management of women with asthma.
Obese people may have a reduced response to inhaled corticosteroids compared with non-obese people, with these medications taking longer to be effective, and with higher doses required for asthma control (Thompson et al. 2021)
The risk for exacerbations is also increased in overweight and obese pregnant women compared to women with a healthy BMI (Murphy et al. 2017, Hendler et al. 2006) one study reported exacerbations requiring medical intervention occurred in approximately one in two overweight and obese women, compared to one in four healthy weight women during pregnancy (Murphy et al. 2017). Although further research is needed to explore the underlying causes, it is has been suggested that the activation of particular immune cells (macrophages) may be involved (Murphy et al. 2017). In addition, lung function – specifically FVC – may be further reduced in the pregnant woman with asthma who is also obese, compared to a woman with asthma of a healthy weight (Jensen et al. 2021).
BMI classifications
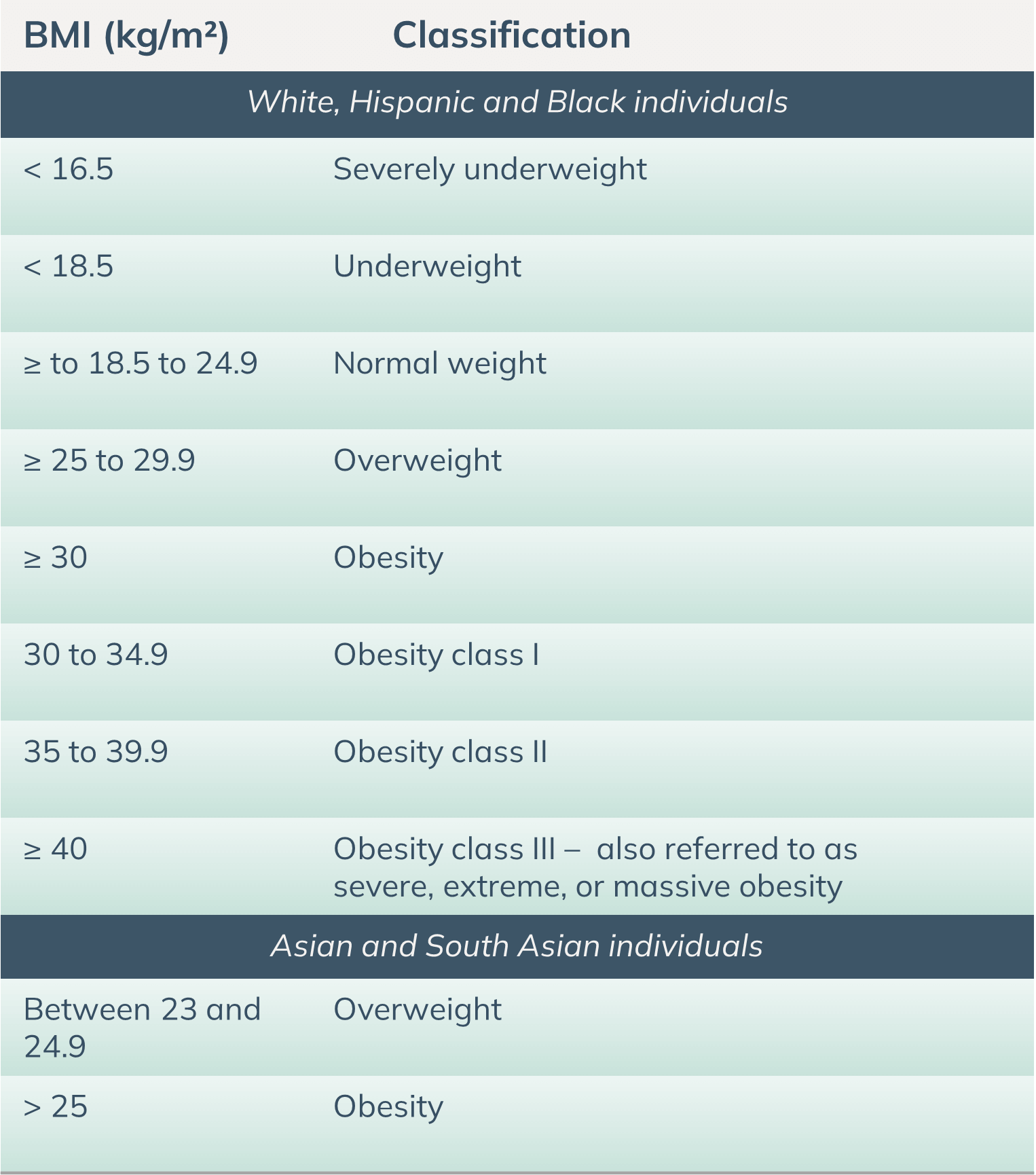
World Health Organization BMI classifications (2000 & 2004)
Calculate BMI
You can calculate BMI using the AIHW BMI calculator found here (which uses WHO classifications for White, Hispanic, and Black individuals. For Asian and South Asian population, please refer to the table above).
Gestational Diabetes Mellitus
Overweight and obesity are strong determinants of GDM. A meta-analysis of 20 cohort studies found that compared to women with a health weight range BMI, those with overweight, obesity and severe obesity were 2, 4 and 8 times more likely to have GDM respectively (Chu et al. 2007).
GDM is a result of insufficient β cell production of insulin to counteract the pregnancy-induced insulin resistance and rise in blood glucose levels. It is diagnosed exclusively in pregnancy and usually resolves following birth. Global estimates place the incidence of GDM at 14% of pregnancies, responsible for the majority of live births affected by diabetes. GDM is associated with an increased risk of poor maternal and infant outcomes, including macrosomia, neonatal hypoglycaemia and premature birth (Jensen et al. 2021).
Maternal asthma is associated with an increased risk of gestational diabetes (Wang et al. 2014, Friedman et al. 2022), with women with moderate to severe asthma at greater risk than women with mild asthma (Wang et al. 2014). The association between maternal asthma and GDM may be driven by metabolic changes and/or risk factors that are common to both conditions, notably obesity and excess gestational weight gain (Jensen et al. 2021). Importantly, a summary of the existing literature suggested that active asthma management (where investigators were involved in the asthma management of women in the study) may remove this increased risk of GDM observed in women with asthma (Wang et al. 2014). Therefore, current evidence points to optimising asthma management, as well as managing lifestyle behaviours, during pregnancy to maintain euglycemia and potentially reduce the risk of GDM development.

Recommendations for management of gestational diabetes and obesity
It is unclear whether the general recommendations for the management of gestational diabetes or obesity should be modified in the presence of maternal asthma. Until this is clarified by further research, it is suggested that the management for obesity and gestational diabetes for pregnant women with asthma follows current clinical guidelines. Additional considerations are as follows:
Encourage women to complete GDM screening
ADIPS Consensus Guidelines for the Testing and Diagnosis of Gestational Diabetes Mellitus in Australia
Monitor gestational weight gain
Monitor where possible to keep within recommended range.
Monitoring of asthma symptoms and treatment effectiveness
Current evidence indicates that an elevated risk of GDM is no longer present when asthma is actively managed. Therefore, monitoring and treatment adjustment as per clinical guidelines are recommended to maintain asthma control during pregnancy, as well as potentially reduce the risk of GDM development. This is particularly important for women with moderate to severe asthma, whose risk of GDM appears even greater than women with mild asthma.
With regards to overweight and obesity, close monitoring of treatment effectiveness is warranted as evidence suggests that some treatment modalities may not be as effective at reducing the incidence of exacerbations during pregnancy.
Corticosteroids for asthma management
Overweight and obese pregnant women who require oral corticosteroids for asthma management require glucose monitoring and consideration of short-term insulin therapy to prevent hyperglycemia. Women with additional known risk factors for GDM (for example previous GDM pregnancy, family history of diabetes/GDM, at risk ethnicities) may also require such considerations if receiving systemic corticosteroid treatment.
Aspirin
The risk of pre-eclampsia is increased in the presence of obesity and gestational diabetes. If low dose aspirin is being considered for pre-eclampsia prevention, the presence of aspirin sensitive asthma should be determined and consultation with respiratory colleagues is encouraged.
Sleep & Reflux
Women with GDM and/or obesity are more likely to experience gastroesophageal reflux and obstructive sleep apnoea. Given these conditions can contribute to worsening asthma symptoms, it is important to be vigilant about the appropriate management of these conditions using behavioural, device and/or pharmaceutical strategies as necessary.
Multidisciplinary team management
Underlying issues to consider with respect to obesity, GDM and asthma potentially include mental health concerns, adverse childhood experiences or other psychosocial concerns/issues, dietary patterns and nutritional intake, physical inactivity, genetics and stress. A comprehensive assessment of dietary, metabolic, respiratory and mental health should follow.
Adjunct therapies to the clinical management of the pregnant woman with asthma may include nutrition therapy, exercise physiology, endocrinology/specialist diabetes teams and psychosocial support. Early nutrition intervention, coupled with appropriate and safe exercise recommendations, is indicated in pregnant women with asthma presenting with overweight/obesity or GDM. Referral to an Accredited Practicing Dietitian can provide tailored nutrition advice and support throughout pregnancy. There needs to be a low threshold for referral for psychological care and social support services.
Breastfeeding
Breastfeeding is an important approach to reducing the risk of the development of type 2 diabetes after gestational diabetes (Gunderson et al. 2015) and for postpartum weight management. Women with GDM and women with obesity may also face additional challenges with breastfeeding (Manerkar et al. 2020, Kozhimannil et al. 2014, Huang et al. 2019) and women with asthma may encounter their own unique challenges. Therefore, encouraging and supporting breastfeeding is particularly important in women with GDM and/or excess weight, and asthma. Referral to a Lactation Consultant and/or an experienced Accredited Practicing Dietician can provide important individual assistance/support/guidance.
Postpartum Metabolic Follow Up
Given the increased rate of type 2 diabetes in women who develop gestational diabetes, and the higher risk of type 2 diabetes in people with asthma and those with obesity it is critical to undertake appropriate follow up post-partum screening for type 2 diabetes, as well as and weight and dietary management.
