It can be challenging to differentiate between physiological and pathological dyspnoea in pregnancy. The issues here are differentiating the effects of pregnancy from those of asthma, and the confusion around words we use to describe difficulty breathing.
During pregnancy it is normal to become more aware of breathing. This can be awareness of increased effort and/or an increased rate of breathing. These changes occur due to the hormonal changes of pregnancy and the mechanical changes of an expanding uterus. While these changes may be noticed they are not usually felt as uncomfortable or distressing. This sensation can be described as ‘shortness of breath’ or ‘breathlessness’.
Breathlessness is common during pregnancy and can occur in up to 70% of healthy women, starting as early as the first trimester (Weinberger et al. 1980, Kikuchi et al. 1994). The perception of breathlessness has been shown to correlate well with the respiratory drive (Kikuchi et al. 1994, Garcia-Rio et al. 1996, Wood et al. 1965). One study showed that healthy pregnant women with breathlessness had a heightened respiratory drive when responding to serum CO2 and hypoxia. Thus it seems that a heightened respiratory drive in pregnancy may contribute to the perception of breathlessness (Garcia-Rio et al. 1996).
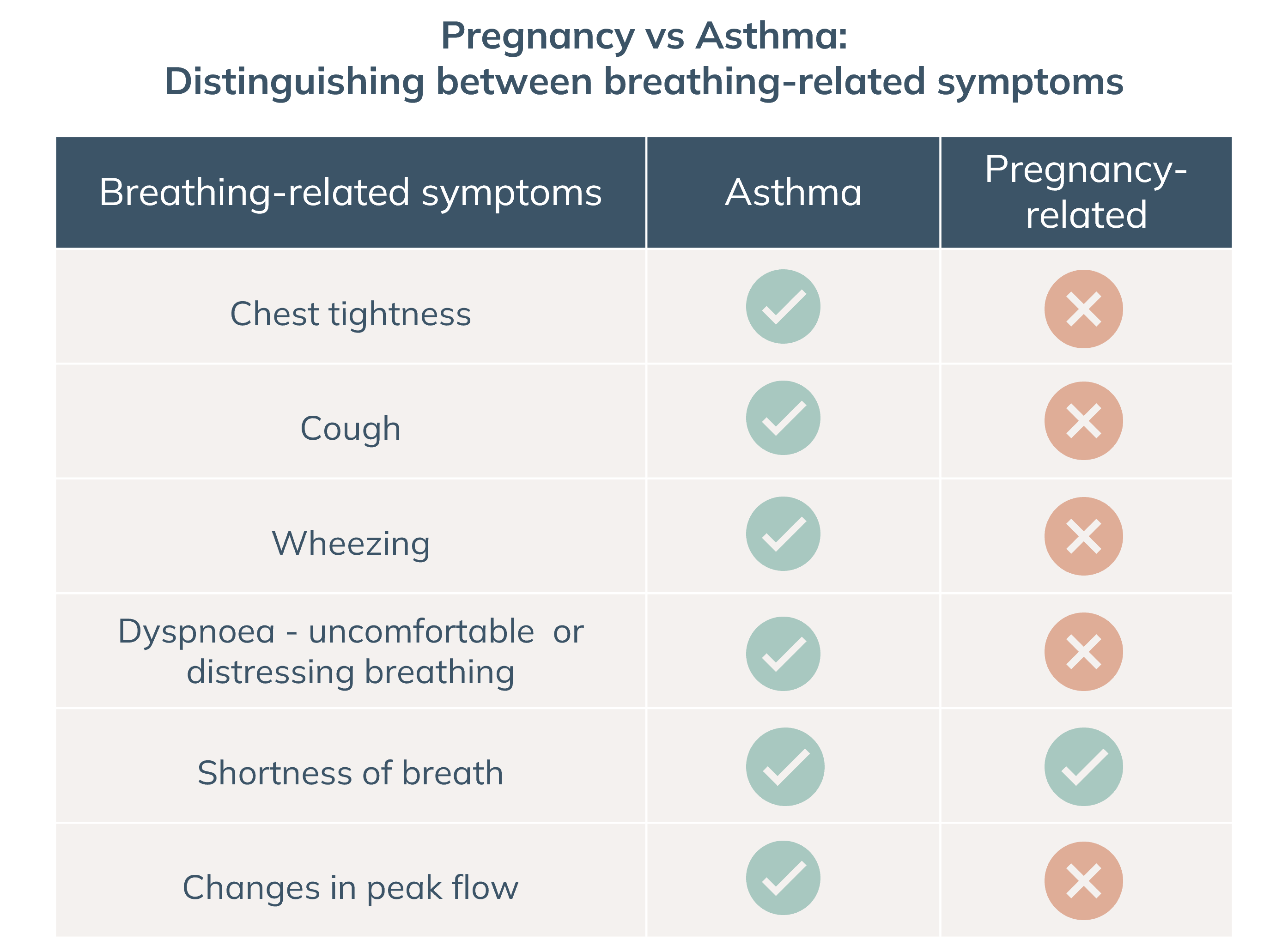
When breathing becomes uncomfortable or distressing, this is referred to as dyspnoea. Asthma often causes dyspnoea while pregnancy regularly causes shortness of breath. Confusion arises because people use the same words to describe breathlessness and dyspnoea and because the common term to describe dyspnoea is also ‘short of breath’, or ‘breathless’. During pregnancy, women with asthma need to recognise whether breathing changes are due to asthma or pregnancy.
Key differences between asthma and shortness of breath due to pregnancy:
- Asthma is usually associated with chest tightness, cough, and/or wheezing whereas shortness of breath due to pregnancy is not.
- Shortness of breath during pregnancy is not associated with changes in peak flow or other measures of pulmonary function. Abnormal spirometry should prompt an evaluation of possible respiratory disease (Hegewald and Crapo 2011).
The AAAAI (American Academy of Asthma, Allergy and Immunology) has developed a modified, validated version of the asthma control test, the P-ACT (Download here) which assesses shortness of breath due to asthma, to differentiate dyspnoea due to asthma and pregnancy (Palmsten et al. 2016).
