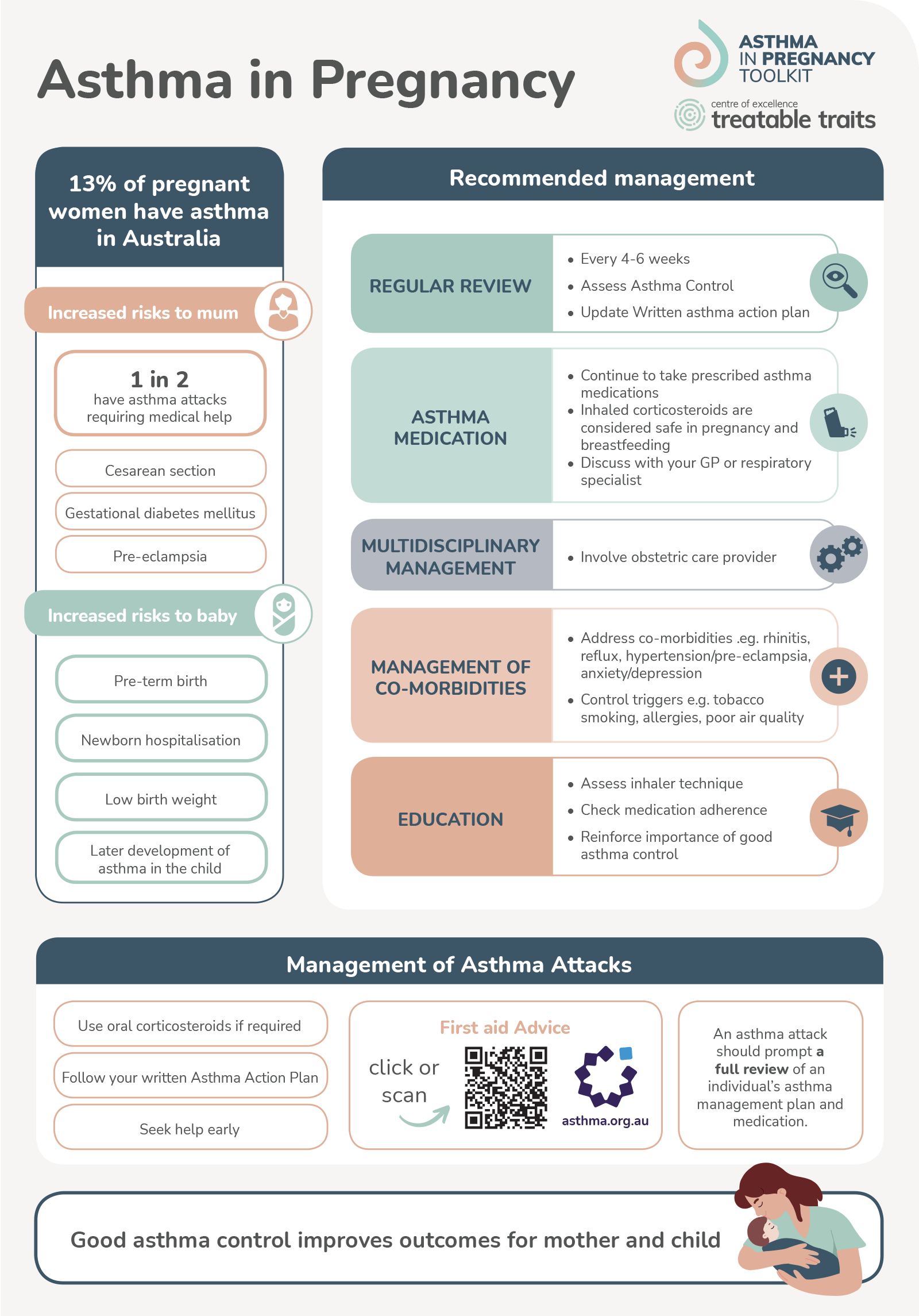
Overview
Asthma is the most common medical condition to affect pregnancy, and exacerbations (asthma attacks) are associated with adverse maternal and perinatal outcomes such as preterm birth and low birth weight. Having good asthma control during pregnancy, reduces the risk of such outcomes.
The frequency and severity of asthma symptoms can change compared to pre-pregnancy. Approximately 30-40% of women may find their asthma worsens during pregnancy so it is important that symptoms are closely monitored throughout pregnancy (Gluck & Gluck 2006, Grosso et al. 2018, Stevens et al. 2022).
Key Messages
- Good asthma control during pregnancy reduces the risk of adverse maternal and perinatal outcomes including: preterm labour and birth, neonatal hospital admission, and gestational diabetes.
- Good asthma control during pregnancy can also reduce the risk of the child developing asthma.
- Monitoring of asthma during pregnancy is important because asthma symptoms can change during this time.
- Asthma self-management skills among pregnant women are low:
- Device technique
- Medication knowledge
- ICS use
- Written Asthma Action Plan possession
- Asthma symptoms, and their response to asthma treatment, during pregnancy are similar to asthma occurring outside of pregnancy.
- Shortness of breath during pregnancy is common, but women with asthma need to be able to differentiate this from asthma symptoms.
- Recognition and management of asthma attacks during pregnancy is the same as in non-pregnant women with asthma, including the use of oral corticosteroids when required.
- Up to 1 in 2 pregnant women with asthma can experience a significant asthma exacerbation for which they may be at greater risk of hospitalisation.