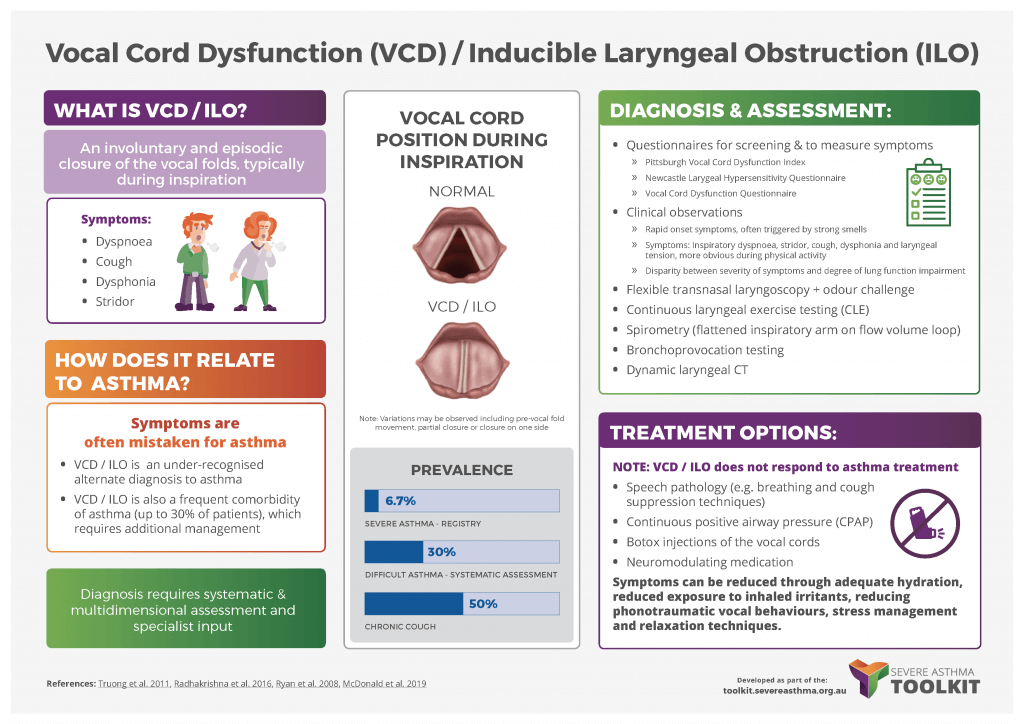
What is VCD?
Vocal Cord Dysfunction (VCD) can be defined as “involuntary and episodic closure of the vocal folds during inspiration which leads to symptoms of dyspnoea, cough, dysphonia, and stridor”. Vocal Cord Dysfunction has been referred to by many different names in the literature. It is commonly referred to as “paradoxical vocal fold movement” (PVFM) or “inducible laryngeal obstruction (ILO)”. VCD is part of the spectrum of laryngeal dysfunction which includes chronic cough, muscle tension dysphonia and globus pharyngeus.
VCD usually occurs during inspiration, but may also occur during expiration. It may be accompanied by a sensation of choking and suffocating, throat or chest tightness. Symptoms are often triggered quickly and resolve quickly once the triggering stimulus is removed.
VCD should be considered when other respiratory causes for symptoms are excluded or are insufficient to explain the severity of the condition or when symptoms are localised to the larynx.
Differential diagnosis includes: asthma, anaphylaxis, laryngeal spasm and subglottic stenosis.
- In contrast with asthma, symptoms in VCD are often localised to the larynx, there is more difficulty with inspiration than expiration, and onset and resolution of dyspnoea episodes is rapid rather than sudden. VCD may co-exist with asthma or may be misdiagnosed as asthma. Symptoms of VCD can mimic asthma leading to an incorrect diagnosis of asthma and escalating treatment of asthma including inhaled and systemic corticosteroids.
- Subglottic stenosis usually results in increased symptoms during exercise.
- Voice symptoms can occur in asthma in the absence of VCD.
- VCD commonly co-occurs in chronic cough (Shembal et al. 2017)
Learn more about VCD and asthma in this infographic from the Severe Asthma Toolkit.
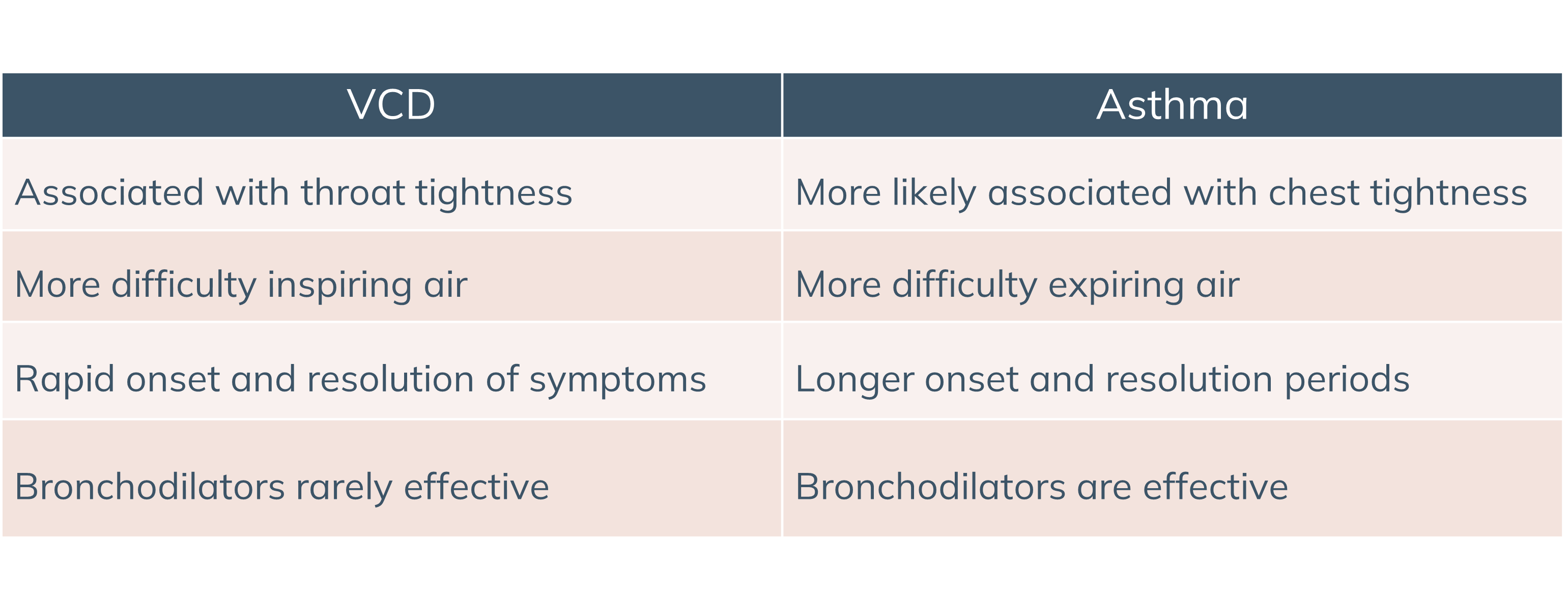
How does VCD differ from asthma?
VCD can be misdiagnosed as asthma. It can co-occur with asthma. Worsening VCD symptoms can sometimes be misattributed to VCD.
Some differences are indicated in the table below:
How is VCD diagnosed?
Pittsburgh Vocal Cord Dysfunction Index
The PVCDI can be used to raise the clinical suspicion of VCD. The PVCDI assesses symptoms of throat tightness, dysphonia, absence of wheeze and triggering by odours as key features that differentiate VCD from asthma. A score ≥4 indicates a diagnosis of VCD (Traister et al. 2014).
Questionnaires
Questionnaires do not diagnose VCD but can measure symptoms associated with VCD.
- Dyspnoea Severity Index
To assess upper airway symptoms and treatment follow-up (Gartner-Schmidt et al. 2014). Score > 10 suggestive of abnormal upper airway dyspnoea. Good reliability and discriminant validity reported, but has not been reported as a diagnostic tool and not specific for VCD. For access email: gartnerschmidtjl@upmc.edu
- Newcastle Laryngeal Hypersensitivity Questionnaire (LHQ)
For the identification of laryngeal dysfunction and to monitor response to treatment (Vertigan et al. 2014). A score of <17.1 is suggestive of abnormal laryngeal function.
Download the LHQ and accompanying Questionnaire worksheet here.
- Leicester Cough Questionnaire
The Leicester Cough Questionnaire is a 19 item scale which measures cough quality of life. It is useful in VCD as symptoms of cough frequently co-occur with VCD and assessment of cough provides a good picture of the patient’s symptom profile.
Clinical observations
Clinical observations include inspiratory dyspnoea, stridor, cough, dysphonia, and tension in the laryngeal region. These symptoms may be absent during quiet breathing but more obvious during physical activity or voice testing. There may be a disparity between pulmonary function testing and symptoms. For example, a patient may have normal baseline spirometry (FEV1, FVC, FEV1/FVC ratio) in the presence of symptoms of breathlessness. Inhaled bronchodilators are frequently ineffective in relieving symptoms or only effective if used in large doses (e.g. 6-8 puffs at a time). Again these observations do not diagnose VCD but they raise the clinical suspicion of VCD.
Functional transnasal laryngoscopy
Laryngoscopy allows visualisation of the vocal folds during quiet respiration, phonation, exercise and odour challenge. Functional laryngoscopy is best when combined with a provocation challenge. Closure (either full or partial) of the true vocal folds is observed during inspiration and may occur more than 50% on expiration. Supraglottic structures such as the false vocal folds may also demonstrate medial and/or anterior/posterior constriction. The larynx may appear normal at rest and provocation through irritant exposure or exercise is needed to observe symptoms (Halvorsen et al. 2017).
The videos below are of flexible transnasal laryngoscopy demonstrating A) normal and B) paramedian vocal folds during expiration, suggestive of VCD.
Laryngoscopy videos
Videos from the Severe Asthma Toolkit.
Content has been reproduced with permission from the Centre of Excellence in Severe Asthma, originally developed as part of the Centre of Research Excellence in Severe Asthma (https://toolkit.severeasthma.org.au).
Flow volume curve
These typically show normal expiratory flow, but the inspiratory limb of the flow volume loop may be flattened. May also indicate a reduction in FIF50 of >20-25% (Sterner et al. 2009, Kenn et al. 2011).

Representative flow volume loop with flattened inspiratory curve (black arrow) following methacholine challenge. Reproduced with permission of the © ERS 2022: European Respiratory Journal Jan 2011, 37 (1) 194-200; DOI: 10.1183/09031936.00192809 (Kenn et al. 2011).
Bronchoprovocation tests with inspiratory loops
Tests using hypertonic saline, methacholine or mannitol may be used. Mannitol has been reported as both a laryngeal provocation agent and bronchial provocation challenge agent in a small case series. The relationship between bronchoprovocation testing and VCD is complex and not completely understood (Tay et al. 2017).
Diagnosis of VCD in pregnancy
There is limited literature about the diagnosis of VCD in pregnancy. Diagnostic procedures would follow the usual procedures for VCD. The exceptions are that the use of co-phenylcaine for laryngoscopy is not recommended. Laryngoscopy can be conducted without co-phenylcaine with patient reassurance. It is recommended that multidisciplinary team discussion occur before proceeding with laryngoscopy. Laryngeal CT would not be recommended. Clinicians should be aware that VCD associated with significant cough could exacerbate incontinence.
How is VCD treated?
- Speech pathology treatment is the mainstay of intervention. It contains several components including:
- Education on what VCD is, how it coexists with asthma and why it needs a different approach to asthma treatment
- Reducing laryngeal irritation by reducing exposure to laryngeal irritants, desensitisation, hydration and reducing phonotraumatic vocal behaviours (Boris et al. 2002)
- Symptom control exercises such as PVFM release breathing. Exercises are timed with asthma medication.
- Psychoeducational counselling
- Inspiratory muscle training
- Treatment of co-existing laryngeal issues such as cough, globus and dysphonia. See infographic below.
